Psoriatic Arthritis Doctor in Clermont: Understanding Symptoms, Risks, and When to Seek Care
If joint pain and psoriasis flares are starting to affect daily life, early rheumatology care can help protect joints and restore comfort.
Important: This page is educational and does not replace medical advice. If symptoms are severe (rapid swelling, fever, chest pain, sudden eye pain/vision changes), seek urgent care.
Psoriatic arthritis (PsA) can feel quiet at first—then suddenly interrupt walking, typing, sleep, and energy. Many people with psoriasis never develop PsA, but it’s common enough that new joint symptoms should be taken seriously, because around 30% of people with psoriasis develop psoriatic arthritis at some point.
This guide explains early signs, who’s at risk, how PsA differs from other arthritis types, and which treatment pathways tend to work best—so the next step is clear and calm.
Understanding Psoriatic Arthritis Quietly
Psoriatic arthritis is an inflammatory arthritis linked to psoriasis, meaning the immune system drives inflammation that can affect joints, tendons, ligaments, and sometimes the spine.
It often develops after psoriasis appears, but symptoms can show up in different orders—so new joint pain in someone with (or with a family history of) psoriasis is worth checking.
What quiet PsA can look like
- Morning stiffness that eases later in the day, then returns after sitting.
- One or two swollen fingers/toes that come and go.
- Heel, bottom-of-foot, or elbow pain where tendons attach to bone.
- Nail pitting, lifting, or new nail changes alongside joint symptoms.
Common First Signs to Watch
PsA can present differently from person to person, but there are classic “clues” that raise suspicion—especially when psoriasis is present.
Early signs that deserve an evaluation
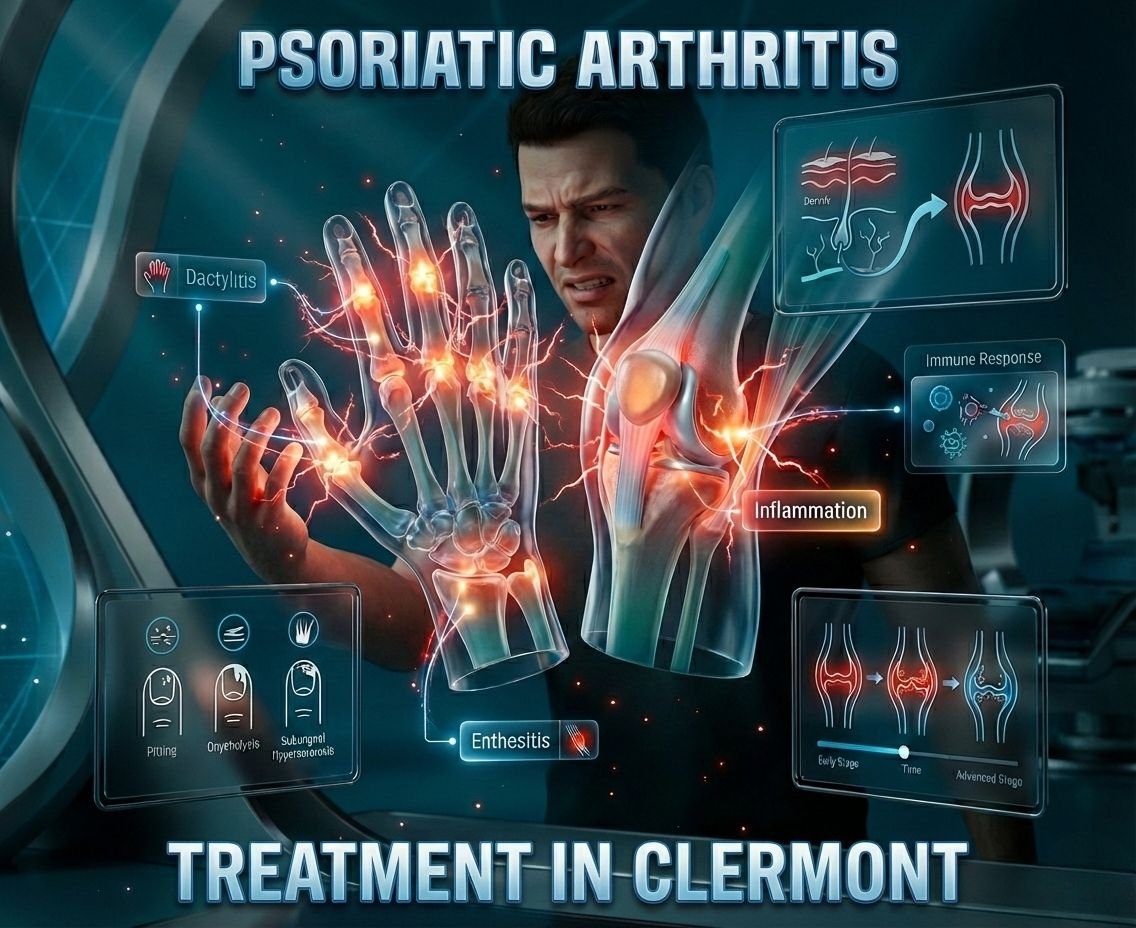
- Dactylitis: Sausage-like swelling of an entire finger or toe.
- Enthesitis: Pain where tendons/ligaments attach (heels, Achilles, plantar fascia, elbows).
- Persistent morning stiffness often 30+ minutes.
- Nail pitting, crumbling, or lifting from the nail bed.
- Back/hip stiffness that improves with movement (possible inflammatory/axial symptoms).
- Fatigue that doesn’t match sleep or workload.
If these symptoms appear in cycles (better for weeks, worse for days), that pattern can still represent inflammatory disease—not just “overuse.”
Who Gets Psoriatic Arthritis?
Psoriatic arthritis can occur at any age, but it typically starts in adults between ages 30 and 55.
Having psoriasis is the strongest risk factor, and family history (parent/sibling) increases risk as well.
Risk factors that may raise concern
- Current or past psoriasis (even mild plaques).
- Family history of psoriatic arthritis.
- New nail changes (pitting, lifting) along with joint pain.
- New inflammatory back pain or recurring tendon pain.
Learn more about Rheumatology Care Associates, or meet the doctor here: Dr. Priya Prakash.
Why Psoriatic Arthritis Feels Sneaky
PsA can fluctuate—some days feel normal, then inflammation ramps up without an obvious injury. This “on/off” pattern often causes people to delay evaluation. Psoriatic arthritis often goes through cycles (flares and remissions).
Why waiting can be risky
- Inflammation can affect joints and tendon attachments even when pain is tolerable.
- Symptoms can shift locations (hands one month, heel the next), which makes it feel less real.
- Psoriasis flares may distract attention from joint warning signs.
Psoriatic Arthritis vs. Other Forms
Several conditions cause joint pain, but psoriatic arthritis is unique because it is associated with psoriasis and can involve nails, tendon attachments, and different joint patterns. Psoriatic arthritis can affect joints and other connective tissue (tendons/ligaments).
| Condition | Common Pattern | Helpful Clue |
|---|---|---|
| Psoriatic arthritis (PsA) | Inflammatory pain; can be asymmetric; can involve spine/tendons | Psoriasis, nail changes, dactylitis/enthesitis. |
| Osteoarthritis | Wear-and-tear pain; often worse with activity | Less swelling from inflammation; no psoriasis link. |
| Rheumatoid arthritis (RA) | Inflammatory pain; often symmetric small joints | Different clinical/lab pattern; not driven by psoriasis. |
Treatment Pathways What Works Best
Treatment depends on which domains are involved (joints, skin, spine, tendons), severity, and overall health, but treatment options for psoriatic arthritis are strong and often life-changing when started early.
Guidelines emphasize short-term NSAID use only for mild PsA and rapid escalation to DMARDs/biologics when targets aren’t met to protect long-term function.
A practical treatment ladder typical flow
- Relief layer: NSAIDs may help pain and stiffness in mild/short-term situations.
- Control layer: Conventional DMARDs (often methotrexate) are recommended quickly for peripheral arthritis in many patients.
- Targeted layer: Biologic DMARDs are used when targets aren’t met; skin involvement can guide choices toward IL-17 or IL-23 pathways.
- Next-step options: JAK inhibitors may be considered—often after biologic failure or when biologics aren’t appropriate, with risk factors weighed.
If you want to explore this topic in detail
Make Sure You Vist This Page By Clicking on This Link To Get In Depth Perspective Upon PsA In Easy Words.
For appointments, use Contact Us.
Why Choose a Rheumatology Specialist?
Psoriatic arthritis is not “just joint pain”—it can involve joints, tendon/ligament attachment points (entheses), skin, nails, and sometimes the spine, so evaluation often benefits from rheumatology expertise.
Specialists also follow evidence-based pathways for escalating treatment when goals aren’t met, including the 2023 EULAR pharmacologic recommendations (published 2024).
What a rheumatology-focused approach adds
- Full domain check: peripheral joints, enthesitis, dactylitis, spine symptoms, skin and nails.
- Targeted treatment strategy: NSAIDs only short-term for mild disease; rapid DMARD start for peripheral arthritis; biologics if target isn’t met.
- Medication selection influenced by psoriasis severity and related conditions (for example, uveitis or inflammatory bowel disease can influence choices).
Meet the doctor here: Dr. Priya Prakash.
Dr. Priya Prakash Leading Clermont Expertise
Patients often look for a steady, methodical plan—clear diagnosis, measurable goals, and a treatment pathway that protects joints while improving day-to-day function.
This blog is structured to help Clermont patients understand PsA patterns and feel prepared for a specialist evaluation, including what to expect and which questions to ask.
Learn more about Rheumatology Care Associates or visit Dr. Priya Prakash.
Care philosophy patient-first and practical
- Listen first, then examine thoroughly: joints, skin/nails, tendon points.
- Confirm the pattern using clinical criteria and appropriate imaging/labs.
- Build a plan that matches severity and lifestyle—not a one-size script.
Why Patients Choose Dr. Prakash
Patients commonly want three things: expertise, clear communication, and a plan that actually fits their life in Clermont.
- Focused psoriatic arthritis experience and structured follow-ups.
- Access to modern therapy options when appropriate, including advanced therapies discussed in current guidelines.
- A calm, thorough evaluation style designed to reduce confusion and delays.
Before your visit, you can explore our Services or review our Clinicians.
Advanced Diagnostics Precision Matters
Psoriatic arthritis can be classified using CASPAR criteria, which require inflammatory articular disease plus at least 3 points from features such as current psoriasis, nail dystrophy, dactylitis, negative rheumatoid factor, and imaging evidence of new bone formation.
Imaging can also help detect inflammation earlier than standard X-rays, and imaging tests and blood tests are commonly used in PsA evaluation.
Tools commonly used to clarify PsA
- Labs: Used to assess inflammation and rule out look-alike patterns; for example, rheumatoid factor testing helps with classification context.
- Ultrasound: Can assess tendons/entheses and detect inflammatory changes; power Doppler can add specificity for active inflammation.
- MRI when needed: Helps assess deeper joints/spine inflammation before changes appear on X-ray.
Note: Classification tools support clinical decision-making but do not replace a full medical diagnosis and individualized evaluation.
Your First Visit What Expect
A first rheumatology visit for suspected psoriatic arthritis typically focuses on your symptom timeline, psoriasis/nail history, a full joint and tendon exam, and deciding which tests are truly necessary.
How to prepare simple checklist
- Bring a list of current medications/supplements and any past treatments for psoriasis.
- Write down the top 3 symptoms to fix first: pain, stiffness, fatigue, skin flares, sleep.
- Note patterns: morning stiffness (minutes), swollen digits, heel pain, flare triggers, and how long flares last.
- If available, bring prior imaging/labs: X-rays, MRI reports, dermatology notes.
What happens in the appointment
- History: joint pattern, skin/nails, family history, and daily impact.
- Exam: joints, entheses (heel/Achilles/plantar fascia), elbows, and digits.
- Plan: confirm working diagnosis, decide tests, and outline a step-by-step pathway.
To request a visit, use Contact Us.
Real Patient Success Stories
Results vary by person, but the goal is consistent: reduce inflammation, protect joints, and help daily life feel normal again.
Mike R., 48 Golfer
Swollen fingers made gripping the club painful and unreliable. After a structured treatment plan and follow-ups, he reported returning to regular play with far less stiffness and improved function.
Sarah L., 39 Teacher
Heel and tendon pain made standing through a school day difficult. With targeted therapy and a guided plan, she reported better stamina and fewer flare interruptions at work.
Reality check: The best outcomes typically come from early evaluation, matching treatment to disease “domains” (joints, skin, tendons, spine), and adjusting until goals are met.
Insurance Cost Reality
Most patients use insurance for rheumatology care, and advanced medications may require prior authorization.
Many plans also allow manufacturer support programs for eligible patients to help reduce out-of-pocket costs for certain specialty therapies.
If you have questions before scheduling, send a message through Contact Us.
Frequently Asked Questions
PsA often shows inflammatory patterns such as morning stiffness, swelling, tendon/heel pain (enthesitis), or “sausage” digits (dactylitis), especially when psoriasis or nail changes are present. Tendon pain, dactylitis, and nail changes are common PsA features.
Yes—most people have psoriasis first, but some develop joint symptoms before obvious skin findings.
Clinicians may use the CASPAR classification approach (inflammatory joint disease plus a point system using features like psoriasis, nail dystrophy, dactylitis, negative rheumatoid factor, and imaging findings).
Guidelines support biologic and targeted therapies when disease is active and treatment targets aren’t met, with medication choice guided by domains involved (skin, joints, spine, enthesitis) and comorbidities.
PsA is chronic, but modern therapies can control inflammation, reduce symptoms, and help prevent joint damage when monitored and adjusted appropriately.
Take Control Today
Psoriatic arthritis can progress quietly, so the most important step is a proper evaluation—especially if joint symptoms are appearing alongside psoriasis or nail changes.
Call to schedule your evaluation, or use online booking to choose a convenient time.
- Phone: (352)-717-0603
- Book online: https://rheumatologycareassociates.com/contact-us/
- Location: 2611 S US Hwy 27 Clermont, FL 34711
Medical note: If symptoms are rapidly worsening, severe, or include eye pain/vision changes, urgent evaluation may be needed.
Or simply reach out here: Contact Us.
Scientific References Guidelines
Sources
- NIAMS Psoriatic Arthritis overview, symptoms, risk factors.
- Mayo Clinic Psoriatic arthritis symptoms/causes, common features like dactylitis and foot pain.
- EULAR recommendations for PsA management (2023 update, published 2024).
- CASPAR criteria publication classification framework.
Return to Rheumatology Care Associates or view About.