Psoriatic Arthritis: Symptoms, Diagnosis & Treatment
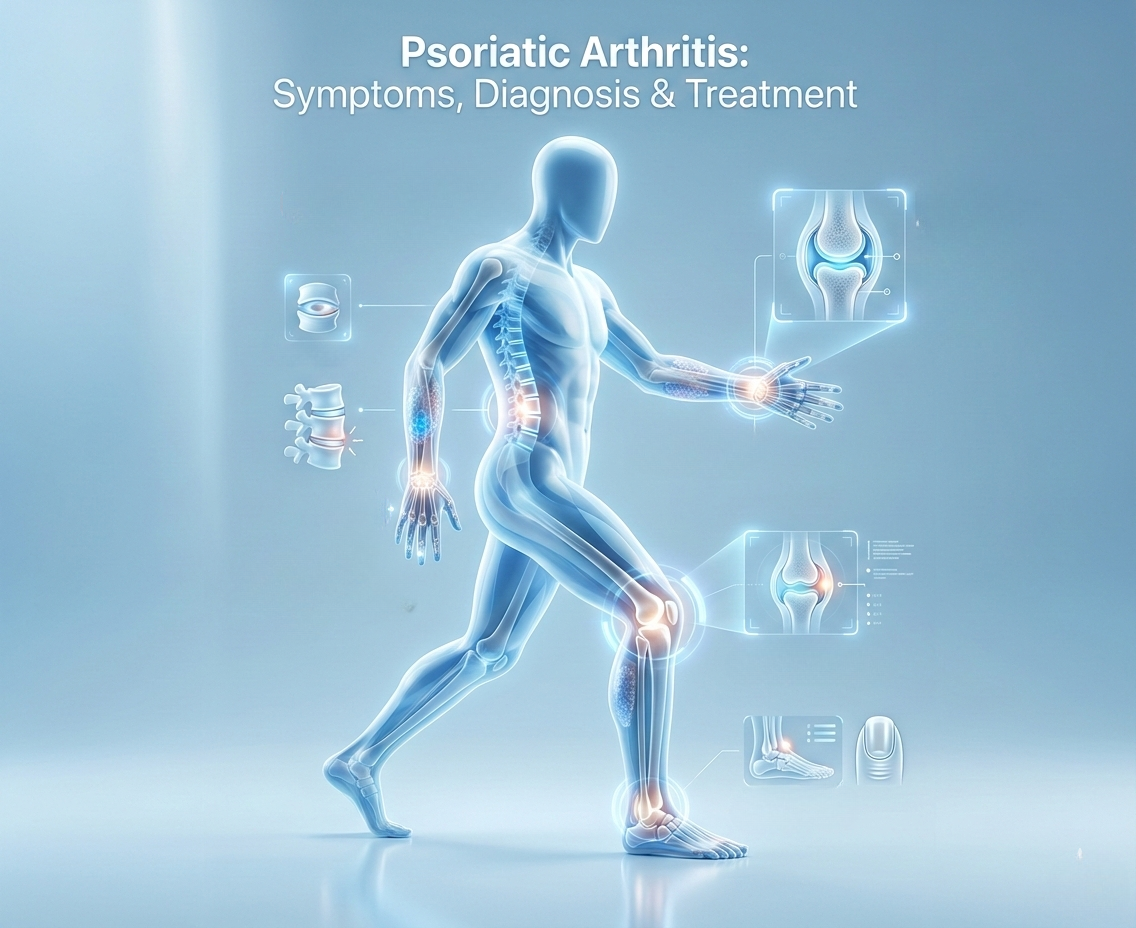
Psoriatic arthritis is a chronic inflammatory joint disease associated with psoriasis that can affect joints, spine, tendons, skin, and nails.
Psoriatic arthritis (PsA) is a chronic inflammatory arthritis linked to psoriasis, affecting joints, skin, nails, and entheses. Accurate diagnosis and consistent management are key to preserving joint function as recommended by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS).
Early inflammation can be subtle, and uncontrolled PsA may lead to irreversible joint damage. This guide explains symptoms, diagnostic criteria, treatment options, and long‑term monitoring based on current guidelines from NIAMS, Mayo Clinic, and EULAR.
If joint pain or stiffness occurs alongside psoriasis, nail changes, or enthesitis, rheumatologic evaluation helps distinguish PsA from other conditions and enables timely, evidence‑based care.
What Is Psoriatic Arthritis?
Types and Patterns of Psoriatic Arthritis
Psoriatic arthritis is an autoimmune form of arthritis that develops in some people with psoriasis. It causes joint pain, swelling, stiffness, and, in some cases, spine or sacroiliac joint involvement according to the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
PsA is not a single disease but a spectrum of patterns, including peripheral arthritis, axial involvement, dactylitis, and enthesitis. Treatment is tailored to the pattern and severity of disease, following published guidelines for inflammatory arthritis.
Why Is Psoriatic Arthritis Often Missed?
Common Diagnostic Challenges
PsA can be overlooked because:
- Early X‑rays are often normalas noted in NIAMS’ guide to psoriatic arthritis diagnosis
- Rheumatoid factor is usually negative
- Symptoms may come and go, mimicking mechanical pain
- Joint, tendon, and spine symptoms overlap with other conditions
A rheumatologist performs a detailed clinical assessment of joints, skin, nails, and entheses to identify PsA even when labs are inconclusive similar to the approach described by Mayo Clinic.
Delayed diagnosis increases the risk of preventable joint damage and functional decline, highlighting the importance of early rheumatologic evaluation.
For a detailed medical explanation of the condition itself, including how it is diagnosed and treated, see our comprehensive guide on psoriatic arthritis symptoms, diagnosis, and treatment .
How Psoriatic Arthritis Is Diagnosed
Clinical Assessment & Examination
Diagnosis relies on clinical evaluation plus imaging and lab tests, not a single positive or negative test. A typical rheumatology evaluation includes:
- Joint count and assessment of tenderness/swelling
- Looking for dactylitis (swollen fingers/toes)
- Checking tendon and ligament insertion points (enthesitis)
- Inspecting skin and nails for psoriatic changes
- Reviewing personal and family history of psoriasis
These findings, combined with imaging and lab tests, are used to classify PsA according to established criteria such as the CASPAR criteria, a widely used classification framework in rheumatology.
How Imaging Helps Detect Psoriatic Arthritis Early
Imaging Modalities for Early Detection
Imaging helps detect active inflammation before permanent joint damage occurs. Standard X‑rays may be normal early, so advanced techniques are often used, as outlined in professional guidelines.
| Modality | Detection Capability |
|---|---|
| Musculoskeletal Ultrasound | Active synovitis, enthesitis, and increased blood flow (Doppler) |
| MRI | Bone marrow edema, early erosions, and sacroiliac joint changes |
Imaging findings support the clinical picture and help guide treatment decisions before irreversible damage develops, consistent with recommendations for early detection of inflammatory arthritis.
Diagnostic Criteria for Psoriatic Arthritis
CASPAR Classification Criteria
Rheumatologists commonly use the CASPAR classification criteria, which require:
- Personal or family history of psoriasis
- Characteristic nail changes (pitting, onycholysis)
- Dactylitis
- Negative rheumatoid factor
- Typical radiographic findings (e.g., erosions, new bone formation)
Meeting enough criteria increases diagnostic certainty, especially in early or atypical presentations. Labs are interpreted in the clinical context, as normal markers do not rule out active PsA, similar to the approach described in NIAMS guidance on psoriatic arthritis diagnosis.
Laboratory Testing in Psoriatic Arthritis
Common Blood Tests & Their Purpose
Blood tests assess inflammation and help differentiate PsA from other conditions, but they cannot diagnose PsA alone. Common tests include:
| Test | Purpose |
|---|---|
| C‑reactive protein (CRP) | General marker of inflammation |
| Erythrocyte sedimentation rate (ESR) | General marker of inflammation |
| Rheumatoid factor (RF) | Typically negative in PsA |
| Anti‑CCP antibodies | Typically negative or low in PsA |
Normal CRP and ESR do not exclude PsA; clinical evaluation remains essential for diagnosis and treatment decisions, as emphasized in Mayo Clinic’s overview of psoriatic arthritis.
Understanding the underlying disease process is essential before selecting therapy. Our psoriatic arthritis overview explains symptoms, diagnostic criteria, and treatment approaches in detail.
How Psoriatic Arthritis Severity Is Assessed
Clinical Indicators of Severity
Severity is determined by:
- Number of inflamed joints
- Presence of spine or sacroiliac joint involvement
- Extent of skin and nail disease
- Functional impact on daily activities
- Imaging findings (erosions, new bone formation)
Earlier and more aggressive treatment generally leads to better long‑term outcomes, with less joint damage and preserved function, as supported by guidelines on psoriatic arthritis management.
How Psoriatic Arthritis Affects the Body
Involvement of Joints, Skin, and Entheses
PsA can involve multiple domains:
- Peripheral joints (hands, feet, knees, etc.)
- Spine and sacroiliac joints
- Entheses (tendon and ligament attachments)
- Dactylitis (swollen fingers/toes)
- Skin and nail psoriasis
Treatment decisions are based on the pattern and burden of disease, aiming to control inflammation across all affected areas, in line with EULAR and ACR recommendations for psoriatic arthritis.
Effects of Untreated or Under-Treated Psoriatic Arthritis
Risks and Complications
- Progressive joint damage and deformities
- Reduced range of motion and functional disability
- Chronic pain and fatigue
- Increased risk of cardiovascular disease and metabolic syndrome
Uncontrolled inflammation accelerates structural damage, making early, consistent management crucial for long‑term health and quality of life, as described in Mayo Clinic’s information on psoriatic arthritis complications.
Psoriatic Arthritis Treatment Options
First-Line and Advanced Therapies
Psoriatic arthritis is treated using a stepwise approach that may include anti-inflammatory medications, disease-modifying antirheumatic drugs (DMARDs), biologic therapies, and targeted treatments. Therapy is tailored to disease severity, affected joints, skin involvement, and patient-specific factors, with the goal of controlling inflammation and preventing joint damage.
PsA treatment is not one‑size‑fits‑all. It depends on the pattern of disease, severity, comorbidities, and patient preferences, following guidelines from NIAMS and professional rheumatology societies.
First‑line options often include NSAIDs for symptom relief. Conventional synthetic DMARDs (e.g., methotrexate, leflunomide, apremilast) are used for moderate disease. For more severe or refractory disease, biologic DMARDs and targeted synthetic DMARDs are commonly prescribed, as outlined in treatment guidelines for psoriatic arthritis.
Treatment selection follows current guidelines and is guided by clinical assessment and monitoring of disease activity, with the goal of minimizing joint damage and preserving function.
Treat‑to‑Target Approach in PsA
Key Steps in Treat-to-Target
Treat‑to‑target means adjusting therapy until a defined goal (low disease activity or remission) is reached. This approach typically includes:
- Regular assessment of joint counts, pain, and function
- Objective measures of inflammation (e.g., composite scores, labs, imaging)
- Treatment escalation or switching when targets are not met
- Shared decision‑making between patient and rheumatologist
Consistent follow‑up helps maintain disease control and minimize joint damage over time, consistent with EULAR and ACR recommendations for psoriatic arthritis management.
How Psoriatic Arthritis Is Monitored Over Time
Recommended Monitoring Practices
Long‑term management requires ongoing monitoring to detect changes early and adjust therapy as needed. Monitoring typically includes:
- Review of symptoms and patient‑reported outcomes
- Joint assessment during physical examination
- Laboratory tests (inflammatory markers if needed)
- Imaging (ultrasound, X‑ray, or MRI) when disease progression is suspected
Regular follow‑up supports early intervention instead of waiting for severe flares or irreversible damage, as recommended in guidelines for the management of psoriatic arthritis.
When and How Treatment Is Adjusted
Treatment Escalation & Switching
If disease activity persists or increases, treatment may be adjusted. Common changes include:
- Increasing dose of current medication
- Adding a second DMARD
- Switching to a different class (including biologics or targeted therapies)
- Addressing medication adherence and lifestyle factors
The goal of treatment is ongoing control of inflammation to preserve joint function and quality of life, in line with published treatment strategies for psoriatic arthritis.
Why Consistent Rheumatology Follow‑Up Improves Outcomes
Benefits of Specialist Care
Patients with regular rheumatology care generally experience:
- Less joint damage on imaging
- Better control of symptoms and disease activity
- Improved quality of life and function
Routine follow‑up allows early detection of worsening disease and timely treatment adjustments, which can prevent long‑term disability, as supported by evidence on the role of specialist care in rheumatic diseases.
Managing Flares and Symptom Changes
Flare Management Strategies
Flares of PsA can occur despite effective treatment, often triggered by stress, infection, or medication changes. Key strategies include:
- Recognizing early signs (increased pain, swelling, stiffness)
- Following a pre‑defined plan for symptom management
- Adjusting treatment (either with a short course of stronger therapy or by changing the long‑term regimen)
- Minimizing prolonged inflammation to protect joints
Communication with a rheumatologist helps fine‑tune treatment and prevent flares from becoming severe, as outlined in patient education resources from major rheumatology organizations.
Psoriatic Arthritis and Systemic Health
Associated Health Risks
Chronic inflammation in PsA is associated with increased risk of:
- Cardiovascular disease
- Metabolic syndrome (obesity, high blood pressure, diabetes)
- Mental health conditions (depression, anxiety)
- Sleep disturbances and fatigue
Comprehensive PsA care includes monitoring and managing these associated risks, integrating rheumatologic and preventive health strategies, as recommended in guidelines on the systemic impact of psoriatic arthritis.
Physical Activity in Psoriatic Arthritis Management
Recommended Exercises
Regular, low‑impact activity helps maintain joint function and reduce stiffness. Recommended activities include:
- Walking
- Swimming or water aerobics
- Stationary cycling
- Stretching and range‑of‑motion exercises
Physical therapy can be helpful for joint‑specific limitations, and a rheumatologist can provide guidance on safe, individualized exercise plans, as supported by recommendations on exercise in inflammatory arthritis from NIAMS and professional societies.
Living With Psoriatic Arthritis: Work and Daily Life
Daily Life & Functional Challenges
PsA can affect work, family responsibilities, and daily routines. Common challenges include:
- Difficulty with fine hand tasks and repetitive movements
- Reduced energy and concentration due to fatigue
- Morning stiffness that delays daily routines
Effective medical management and appropriate support (such as ergonomic adjustments, pacing, and medication timing) help maintain independence and quality of life, as described in patient education materials on living with psoriatic arthritis.
The Role of Patient Education in Psoriatic Arthritis
Benefits of Education
Understanding PsA improves self‑management. Patient education helps with:
- Recognizing early warning signs of flare or progression
- Understanding treatment goals and medication options
- Communicating symptoms accurately to the care team
- Setting realistic expectations for disease control
Ongoing education is a standard part of rheumatology care and supports better long‑term outcomes, as emphasized in guidelines on patient education for chronic inflammatory arthritis.
Psoriatic Arthritis Care in Clermont, Florida
For people in the Clermont area, access to a rheumatology practice with experience in psoriatic arthritis can support timely diagnosis and ongoing management. Local care typically includes:
Psoriatic arthritis is one of several inflammatory arthritis conditions managed by rheumatology specialists, alongside rheumatoid arthritis and axial spondyloarthritis.
Local Care Services
- Comprehensive joint–skin–spine assessment
- Access to advanced imaging and lab services
- Onsite treatment options, including biologic and infusion therapies
Long‑Term Psoriatic Arthritis Management in Clermont
Structured Long-Term Management Plan
Psoriatic arthritis is progressive when untreated or under‑treated. Long‑term outcomes depend on continuous monitoring, timely treatment escalation, and consistent follow‑up with a rheumatology specialist.
Before choosing care, it’s helpful to understand the condition itself. Learn more about psoriatic arthritis symptoms, diagnosis, and treatment options in our educational medical guide.
A structured, long‑term plan aims for low disease activity or remission, helping patients preserve joint function, stay active, and avoid preventable disability — key goals for quality of life in psoriatic arthritis.
Learn about long‑term PsA care in ClermontFrequently Asked Questions
Psoriatic arthritis often causes inflammatory joint pain with morning stiffness, swelling, enthesitis (tendon/heel pain), and dactylitis (sausage‑like swelling of fingers or toes). It commonly occurs in people with psoriasis or nail changes, but not always. A rheumatologist can help distinguish PsA from other causes using clinical evaluation, imaging, and lab tests, as outlined in PsA diagnostic guidelines from NIAMS and professional societies.
Yes, in some people, psoriatic arthritis begins before noticeable skin psoriasis. Joint symptoms (like foot, heel, spine, or finger pain) or nail changes may appear first, and skin psoriasis may develop later. A rheumatologist can evaluate this pattern clinically and confirm PsA even when skin disease is not yet obvious, as described in overviews of psoriatic arthritis from major medical centers.
There is no single test that diagnoses psoriatic arthritis. Diagnosis relies on clinical evaluation, imaging (ultrasound or MRI), and laboratory tests. Rheumatologists commonly use the CASPAR classification criteria, which consider personal or family psoriasis, nail changes, dactylitis, negative rheumatoid factor, and X‑ray findings, as detailed in rheumatology guidelines and resources from NIAMS and Mayo Clinic.
Yes, biologics and newer targeted therapies are effective for many patients with active psoriatic arthritis that doesn’t respond adequately to conventional treatments. They work by targeting specific parts of the immune system to reduce inflammation and slow joint damage. Treatment choice depends on disease severity, pattern, comorbidities, and individual factors, as recommended in current treatment guidelines for psoriatic arthritis.
Psoriatic arthritis is a chronic condition and cannot be cured, but it can be controlled. Modern treatments can achieve long‑term remission or low disease activity, preventing joint damage and preserving function. Ongoing monitoring and adherence to treatment are key to maintaining remission and quality of life, as emphasized in patient education materials from NIAMS and major rheumatology organizations.
When to seek medical evaluation: New or worsening joint pain, prolonged morning stiffness, swollen fingers or toes, or joint symptoms occurring with psoriasis or nail changes should prompt evaluation by a healthcare professional.
Next Steps for Psoriatic Arthritis Care
Psoriatic arthritis can progress quietly, so the most important step is a proper rheumatologic evaluation — especially if joint symptoms are appearing alongside psoriasis, nail changes, or enthesitis.
Consider scheduling a rheumatology evaluation if:
- Joint pain, swelling, or stiffness has been present for more than a few weeks
- Morning stiffness lasts more than 30 minutes
- There is a personal or family history of psoriasis or nail changes
Trusted medical sources
Sources
- NIAMS Psoriatic Arthritis overview, symptoms, and disease burden.
- NIAMS – Diagnosis, Treatment, and Steps to Take official guide for patients and clinicians.
- Mayo Clinic Psoriatic arthritis symptoms and causes, inflammatory features including dactylitis and enthesitis.
- EULAR recommendations for PsA management (2023 update, published 2024).
- CASPAR criteria publication, classification framework for psoriatic arthritis.
Care Options for Psoriatic Arthritis
Patients seeking specialized care may also find the following resources helpful:
Medical note: If symptoms are rapidly worsening, severe, or include eye pain/vision changes, urgent evaluation may be needed. This content is for educational purposes only and does not substitute professional medical advice. Diagnosis and treatment decisions should be made in consultation with a qualified healthcare provider.
Last updated: January 2026, Medically reviewed by: This content was written for educational purposes and medically reviewed by a board-certified rheumatologist to ensure accuracy and alignment with current clinical guidelines.
This page is intended as an educational overview of psoriatic arthritis and does not promote a specific treatment or medical provider.
More information on psoriatic arthritis care: Contact Us